
Samples
By Rachel Ann Tee-Melegrito
Immunity definition
Herd immunity
After COVID-19 infection
COVID-19 vaccine
Immunity duration
Does it prevent infection?
Summary
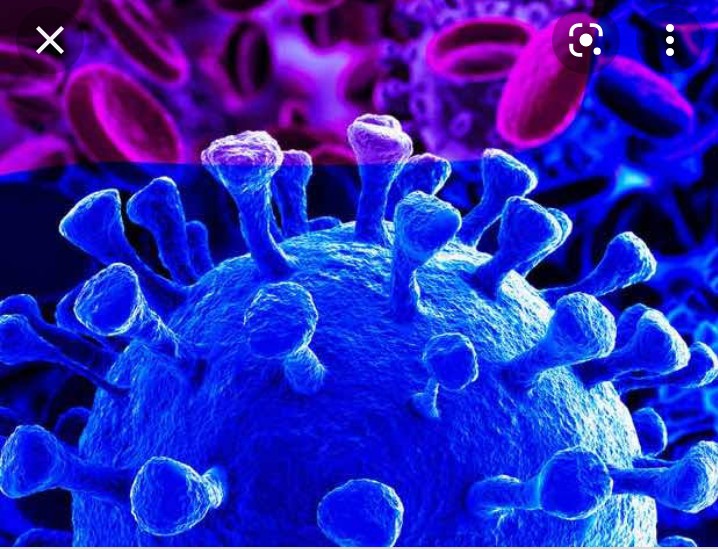
Severe acute respiratory syndrome coronavirus 2, or SARS-CoV-2, is the virus that causes coronavirus disease 19 (COVID-19). To prevent COVID-19, a person requires immunity to the virus. To attain immunity and protection, a person likely needs to either naturally recover from the disease or receive a COVID-19 vaccination.
Vaccination programs are rolling out worldwide to deploy safe and effective vaccines against COVID-19. At present, evidence suggests that roughly one-third of the world’s population have received at least one dose of a COVID-19 vaccine and approximately one-quarter are fully vaccinated.
A person can also develop immunity from COVID-19 following direct exposure to the virus, but this runs the risk of complications from the disease. While there is limited data on the length of immunity, evidence suggests it is a short term effective way to prevent infection. If enough people within a population become immune to a disease, they may achieve herd immunity, which can help protect people who may be unable to receive the vaccine.
In this article, we discuss immunity to SARS-CoV-2, including how to acquire it, how long it lasts, and whether it prevents infection.
What is immunity?

Immunity refers to the body’s ability to protect against and fight off infectious diseases. There are three types of immunity: innate, adaptive, and passive.
Innate immunity
A person has an innate immune system that acts as the first line of defense against pathogens. This refers to barriers, such as the skin and mucous membranes, that prevent harmful substances from entering the body.
Adaptive immunity
Also known as active immunity, this refers to the immune system producing antibodies to a pathogen after exposure to a disease organism. The immune system can recognize the pathogen and quickly produce these antibodies to prevent future infections.
A person can acquire adaptive immunity through natural exposure to the pathogen, known as natural immunity, or introduction to an inactive portion of the pathogen through a vaccine, reffered to as vaccine-induced immunity. Either way, a person can produce a suitable immune response that is long lasting and sometimes lifelong.
Passive immunity
Passive immunity is when a person receives antibodies to a disease rather than producing them through their immune system. For example, a newborn infant can receive passive immunity through the placenta, or a person can receive passive immunity through antibody-containing blood products.
This can be useful as passive immunity provides immediate protection, while adaptive may require weeks to develop. However, while adaptive immunity is long lasting, passive immunity typically only lasts for a few weeks or months.
Herd immunity
Herd immunity, or population immunity, aims to control and prevent disease spread by making a significant portion of the population immune to a contagious disease. The idea is to provide protection by decreasing the number of people susceptible to contracting and transmitting the disease. This indirectly protects people who may not be suitable for a vaccination, including young children and people with certain health conditions.
The percentage of the global population that needs to be immune to achieve herd immunity — called a threshold — varies by disease. Generally, thresholds are only achievable with high vaccination rates. While the herd immunity threshold is not known for COVID-19, evidence suggests it may require roughly 70% of the population to be immune to the disease.
While vaccination rates are increasing, some evidence suggests that factors such as vaccine hesitancy, the emergence of new variants, vaccine delays for children, and continuing transmission may make herd immunity slightly harder to achieve.
Immunity after COVID-19 infection
People previously infected with COVID-19 develop natural immunity against the disease. Their immune system can recognize SARS-CoV-2 and immediately produce antibodies to fight off an infection. After identifying a pathogen, the immune system keeps special white blood cells — called memory cells — that go into action quickly to fight the infectionTrusted Source if the body encounters the same pathogen.
Evidence from the World Health Organization (WHO) indicates that 90–99% of people with a SARS-CoV-2 infection develop protection against the virus. Individuals typically develop antibodies roughly 3 weeks after a SARS-CoV-2 infection. Research also suggests that people develop a robust adaptive immune response, regardless of their disease severity.
Currently, scientists measure immunity based on the presence of neutralizing antibodies (Nab) in the blood. These antibodies can neutralize the virus by blocking its entry into the cell. A 2020 observational study and a 2021 study found that previously infected individuals develop high titers of Nab, especially those with severe COVID-19 disease.
However, evidence is still unsure of the duration of these antibodies. A 2021 study suggests a possible decline in postinfectious antibody response, which may explain examples of reinfection.
Vaccination

A person who receives a vaccination develops active immunity for the disease the vaccine protects against. Vaccines allow the body to develop an immune response without requiring an infection. All vaccines currently in use produce high titers of neutralizing antibodies. However, a 2021 study suggests that mRNA-based types show the most efficacy.
A 2021 study estimating mRNA vaccine effectiveness among frontline and other essential workers indicate they are 90% effective for those with full immunization regardless of symptom severity and 80% effective for the partially immunized. Another 2021 study compared the duration of in vitro immune protection between vaccines and previous infection based on neutralization titers and found similar results.
In addition to being safer, evidence also suggests that immunity from vaccination produces a stronger and longer lasting immune response. Emerging evidence also suggests that people get better protection from being fully vaccinated than having had COVID-19, indicating that even if a person has recovered from COVID-19, they should still receive a vaccination.
How long does immunity last?
Research into how long people are protected against SARS-CoV-2 is still ongoing, but evidence suggests that immunity could last for several months or a couple of years.
A 2021 study found that previously infected individuals retain immunological memory to SARS-CoV-2, with robust immunity up to 8 months after infection. Another study indicates that people previously infected with COVID-19 who had a vaccine after recovery, receive a boost in immunity and develop some protection from the disease for at least a year.
Another 2021 study identified long-lived antibody-producing cells in the bone marrow of individuals who recovered from COVID-19, indicating that it may be possible for these people to produce antibodies against SARS-CoV-2 for most of their life. However, more evidence is necessary to confirm this.
While there is not as much evidence on the duration of immunity from vaccines, a 2021 study no suggests that vaccination significantly boosts immune activity.
Does immunity prevent infection?
Reports of reinfections are unlikelyTrusted Source but can occur. However, WHO’s scientific brief on natural immunity shows that previous infection provides people with 80–90% protection from reinfection for up to 7 months and about 94% protection from acquiring severe COVID-19.
Similarly, a report from the Centers for Disease Control and Prevention (CDC) showed that one-fourth of the new infections happen in fully vaccinated people. However, they were less likely to require hospitalization or cause severe illness even during the period when the Delta variant is already predominant.
Moreover, a 2021 review found that in recovered and immunized people, those with no previous infection, previously infected but asymptomatic, or infected with mild to moderate cases who developed low levels of acquired immunity, are more likely to get reinfected.
This is consistent with a 2021 study that found those with more severe COVID-19 disease are likely to have a more robust immune response to SARS-CoV-2 and will likely have a higher level of protection from reinfection.
Summary
People can become immune to SARS-CoV-2 through adaptive immunity. This can be through either natural immunity or vaccine-induced immunity. While research is still ongoing, evidence suggests that both provide effective and long lasting immunity. With a high enough vaccination rate, it may still be possible to achieve herd immunity.
While it is still possible to acquire reinfection of the disease or a SARS-CoV-2 infection after a vaccination, adaptive immunity can still provide protection. It is advisable for people to continue practicing protective measures, such as hand washing, physical distancing, and wearing face masks.






