Illustration
Written by Jayne Leonard (MNT)
Types of prostatitis
Causes
Symptoms
Diagnosis
Treatment options
Female prostatitis
Takeaway
Bacteria can infect the prostate, and this may result in inflammation. The medical term for this is bacterial prostatitis. It can cause intense pain and changes in urination.
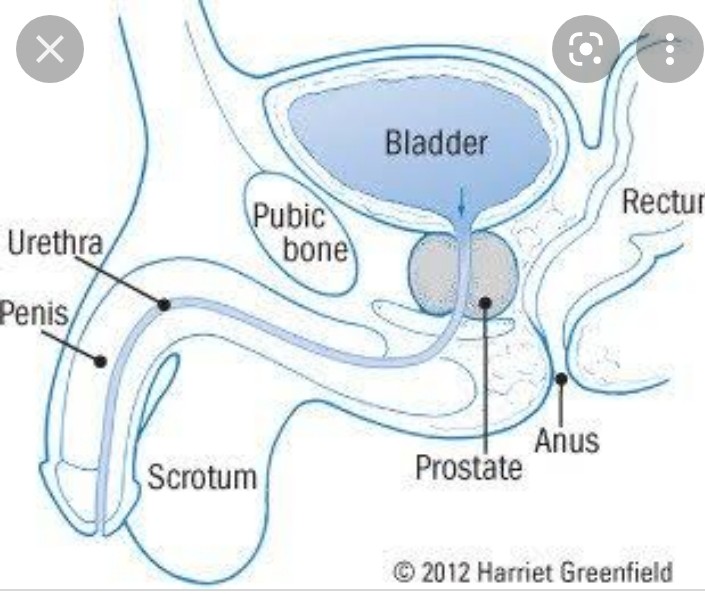
The prostate is a small, walnut-shaped gland that forms part of the male reproductive system. It sits just under the bladder and produces a component in semen. The urethra, a tube connecting the bladder to the penis, passes through the prostate and carries urine.
Prostatitis is a common prostate problem that can cause a variety of symptoms, including pain and difficulty urinating. While there are different causes and types of prostatitis, bacterial infections can often result in inflammation of the prostate.
When the cause is an infection, there are two main types of prostatitis:
Acute bacterial prostatitis
If a person has an acute, or short-term, prostate infection, symptoms are severe, and they develop suddenly.
Prostatitis is the term for inflammation of the prostate. Acute prostatitis is uncommon, and the cause is always an infection.
The infection requires immediate treatment as the condition can cause serious complications.
Chronic bacterial prostatitis
Chronic, or long-term, bacterial prostatitis causes symptoms that tend to come and go over several months.
If an infection is responsible for the inflammation, the medical community calls this condition chronic bacterial prostatitis.
If there is a different cause, the condition is called either chronic prostatitis or chronic pelvic pain syndrome, and it affects 10–15% of males.
What are the causes?
Acute prostatitis results from a bacterial infection. Bacteria from urine may flow backward from the urethra and spread to the prostate gland. If antibiotics do not kill the bacteria, prostatitis may recur and become chronic.
While other causes are less well understood, if a person does not have a bacterial infection, prostatitis may instead result from nerve damage in the lower urinary tract following surgery or trauma or due to the immune system’s response to a previous urinary tract infection (UTI).
Risk factors
Some people are more likely to get prostate infections. Risk factors can include:
using a catheter
an abnormality in the urinary tract
a current bladder infection or UTI
a history of prostatitis episodes
sustained injuries to the pelvis after undergoing procedures involving the urethra or prostate
Symptoms
The signs and symptoms of bacterial prostatitis depend on whether it is acute or chronic.
Acute bacterial prostatitis
Symptoms appear suddenly and are severe. They can include:
urine with an unpleasant odor
blood in the urine or semen
body aches
burning pain while urinating
difficulty urinating
fever or chills
frequent urination
nausea
nocturia (urinating 2–3 times per night)
pain in the lower abdomen or lower back
vomiting
Acute bacterial prostatitis requires prompt medical attention.
Chronic bacterial prostatitis
These symptoms may be mild to moderate and either develop gradually or come and go over several months.
The medical community considers bacterial prostatitis to be chronic if symptoms are present for at least 3 months and include:
an urgent need to pass urine
bladder pain
burning pain during urination
difficulty passing urine
frequent urination
pain in the lower abdomen, back, or groin
pain in the testes or penis
painful ejaculation
a UTI
Diagnosis
To diagnose a prostate infection, a doctor mayTrusted Source:
take a medical history
inquire about symptoms
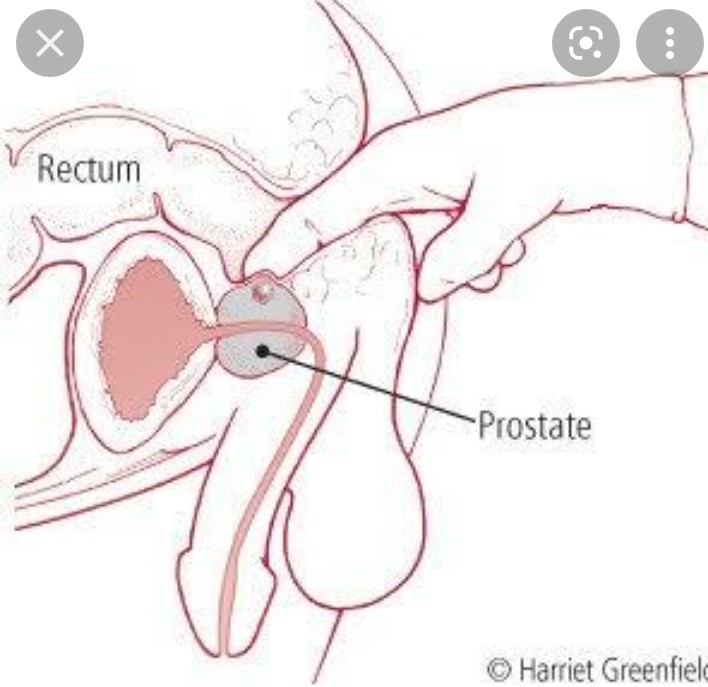
perform a physical examination, including a digital rectal exam
analyze a urine sample for signs of an infection
The doctor may also order one or more of the following:
blood tests to check for signs of an infection or another problem
semen analysis to look for signs of an infection
imaging tests to check for blockages or other issues in the urinary tract or prostate
prostatic massage, which involves massaging the prostate and checking the discharge for abnormalities
a biopsy, which involves taking some tissue from the prostate and examining it under a microscope
These tests can confirm a diagnosis of prostatitis and rule out other conditions, such as prostate cancer.
The results can also help to determine the best course of treatment.
Treatment options
Both medical and natural treatments can help people with prostatitis.
Medication
Medications for prostatitis include:
antibiotics
alpha-blockers
anti-inflammatory medications
To relieve pain and inflammation, some people take nonsteroidal anti-inflammatory drugs, such as ibuprofen, meloxicam, and naproxen. These are available over the counter or by prescription. People may use alpha-blockers as these drugs can relax prostate muscle and make it easier to urinate.
Surgery
Surgery may be necessary, though this is uncommon.
Surgeons can remove blockages or scar tissue from the bladder, which can improve the flow of urine and reduce symptoms of prostatitis.
Natural treatments
Home remedies may help to relieve some symptoms, but they typically cannot eliminate bacteria from the prostate. Medical treatment is usually necessary.
Home remedies can include:
drinking more water to help flush out bacteria
avoiding bladder irritants, such as alcohol, caffeine, and spicy food
soaking in a warm sitz bath
using a heating pad to alleviate pain
avoiding activities that irritate the prostate, including cycling, horseback riding, and anything involving prolonged periods of sitting
practicing Kegel exercises to train the bladder
Some people might also find relief from the following alternative therapies:
acupuncture
biofeedback
herbal supplements, such as ryegrass and saw palmetto
Female prostatitis
The prostate is not typically part of the female anatomy. However, there are a series of glands and ducts at the front of the vagina, known as Skene’s glandsTrusted Source, that some people may refer to as the “female prostate.” While the medical community does not fully understand the role of these glands, older research suggests they may have some similar properties to the male prostate gland.
When a doctor refers to female prostatitis, it may be a reference to an infection of the Skene’s glands. In some cases, sexually transmitted infections, such as gonorrhea, may spread to the female prostate. Alternatively, it may be urethral syndrome, which describes a group of symptoms that occur following irritation of the urethra.
Takeaway
Anyone with symptoms of a bacterial prostate infection should see a doctor immediately.
If a person does not receive treatment, the condition can cause complications, such as:
an abscess in the prostate
bacteremia (a bacterial infection of the blood)
chronic pain
epididymitis (inflammation at the back of the testes)
infertility
urinary problems
To avoid complications and ease symptoms, people should seek prompt medical attention and follow the doctor’s treatment plan.
A person may have to switch to a different antibiotic before seeing results. Also, in some cases, a chronic bacterial prostate infection may only clear completely after months of antibiotic treatment.






